Nokuthaba Dlamini
A huge number of Covid-19 victims in Zimbabwe are dying outside health institutions, before they can access treatment, an analysis of official statistics has revealed.
Zimbabwe’s health delivery system is in danger of being overwhelmed by the resurgent Covid-19 outbreak, which some experts believe is being fueled by the new South African variant of the virus that was first identified in China in 2019.
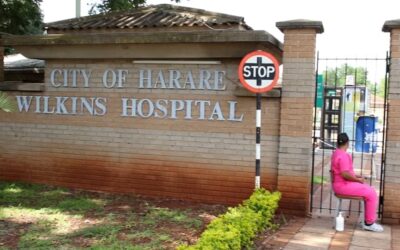
Some Zimbabweans that have fallen seriously ill after contracting the virus have failed to access life-saving treatment because hospitals tend to run out of beds or do not have enough oxygen.
In some parts of the country such as Bulawayo—the epicentre of the pandemic before the shift to Harare during the second wave—there are limited facilities to handle Covid-19 cases as the government is still struggling to upgrade designated hospitals.
Waiting to inhale
Authorities at the United Bulawayo Hospitals, the only operational public health facility for Covid-19 patients in the country’s second largest city, last week warned that oxygen stocks had become dangerously low.
An analysis of Covid-19 statistics tracked by The Standard working in collaboration with Information Development Trust—a non-profit organisation supporting local investigative journalism – revealed that a staggering number of people were dying in the communities.
According to statistics from the Health and Child Care ministry, Harare accounted for 49.1% of Covid-19 deaths that occurred outside hospitals countrywide between March 20, 2020 and January 16, 2021, against a national average of 31.7%.
At least 45.4% of Covid-19 deaths in the capital during the same period happened outside hospitals.
Matabeleland South, at 50% community deaths, however, had the highest provincial proportion of people dying at home.
It was followed by Mashonaland West at 48.1%, Matabeleland North (42.9%) and Mashonaland East (42.1%).
Zimbabwe’s once robust health delivery system has over the years been weakened by gross underfunding and a brain drain that has left major hospitals without equipment and drugs.
The Covid-19 outbreak that began in March last year also coincided with prolonged strikes by health workers, who were protesting against lack of personal protective equipment
and poor working conditions.
Zimbabwe Association of Doctors for Human Rights (ZADHR) executive director, Calvin Fambirai, said the high incidence of community deaths pointed to a serious crisis in the health delivery system.
“This could be indicative of an overburdened health system that is now failing to cope with the disease burden,” Fambirai told The Standard.
“It can also point towards a weak surveillance system where cases are not identified early.
“It may show poor confidence in the health care system as some individuals choose to be treated outside the formal care system,” he added.
Poor testing capacity
Zimbabwe’s Covid-19 testing capacity remains low, with only 3, 829 having taken PCR tests countrywide on Friday, 22 January 2021.
Chitungwiza, a sprawling town with a population of 350 000, conducted a meagre 28 PCR tests on the same day.
Itai Rusike, executive director of the Community Working Group on Health (CWGH), said the second wave of the Covid-19 outbreak that started with the re-opening of borders in December and the influx of returning residents during the festive season had put a severe strain on the health delivery system.
“What has been happening since the country was opened up and the borders, together with the relaxation of the lockdown up to the festive season, our cases have escalated and as a result we have overburdened our hospitals,” Rusike said.
“What we are now seeing is a result of the complacency that has been happening within the generality of our population in terms of the adherence to the Word Health Organisation (WHO) Covid-19 prevention guidelines.
“ It’s not surprising that some people are now beginning to die at home because the cases are increasing. Our hospitals throughout the country are overwhelmed and most of them are at full capacity.
“So it is very common now that some people call the hospitals seeking admission and they are told that the hospitals have no extra beds to offer,” said Rusike.
Some desperate Zimbabweans have been taking to social media appealing for help to secure hospital beds or oxygen for their dying relatives.
Those with resources even offer to pay any amounts of money to secure hospital beds at Covid-19 treatment centres.
Rusike said a significant number of Covid-19 patients have also died while on their way to hospitals because they would have first tried less expensive home remedies.
“What is commonly happening is that some relatives try to drive to the hospitals late and some patients die on the way, some in hospital car parks while others upon admission and this brings a lot of challenges not just to the health sector, but to the communities in terms of the transmission levels,” he said.
“Most of the family members may not be well equipped in terms of protecting themselves from getting Covid-19, so as a result, we are seeing a spike in local transmissions because of the poor management that is happening starting at family level.”
Zimbabwe Nurses Association president, Enock Dongo, said it did not come as a surprise that more people were dying of Covid-19 at their homes as the country’s health delivery system was in shambles.
Home remedies
Dongo said most people suffering from Covid-19 opted to use local herbal and fruit remedies such as lemons, zumbani\umsuzwane leaves and ginger, among other concoctions, to strengthen their immunity.
“Whenever they (patients) go to health institutions, they do not get the help that they are supposed to be getting.
“We do believe in modern medicine, but most of the times drugs are in short supply at public hospitals. In a way, people have become their own nurses and doctors. They are desperate and helpless.”
Rusike and Dongo concurred that Zimbabwe’s response to Covid-19 remained poor nearly a year after the first case was recorded in the country.
“If you look at the number of hospital beds, they are very low and unfortunately our health workers are also being overwhelmed and are not fully protected and, as a result, some have lost their lives,” Rusike said.
The CWGH boss, whose organisation is a network of various groups lobbying for universal access to health, also believes that a large number of Covid-19 deaths are going unreported especially in the remote parts of Zimbabwe.
“Even on the issue of mortality, there a lot of community deaths that are happening in remote communities and some people have been buried without the families knowing that the deaths were Covid-19 related,” Rusike said.
Dongo urged government to allocate more funds to the public health system.
Health and Child Care deputy ministry spokesperson, Donald Mujiri, accused people of failing to cooperate with health workers during contact tracing.
Published as a follow-up collaboration between Information for Development Trust (IDT) and The Standard, as part of the IMS-FOJO ZimMedia21 Project



























































































0 Comments